Welcome back to the second part of the first Mental Health Monday. This time we will be discussing the second leading mental health disorder: depression. Please note that these subjects can be sensitive to some people. *Discretion is advised.*
Depression
Short term depressed moods are experienced by everybody. These are “the blues” and sadness. A major depressive mood disorder lasts for at least two weeks and affects the person’s ability to work, hold relationships and participate in daily activities. Major depressive mood disorders are 6.8% of reported illnesses making them number two in mental health illnesses. The median age is 32 which is much later than anxiety. Depression can occur with anxiety and substance abuse disorders. Unfortunately, people with major depressive mood disorders are prone to the return of the depression. Once again, females are the leading gender affected by this disorder. The most common types of mood disorders include:
- Major Depressive Disorder (often referred to as Clinical Depression) – generalized depressive episodes. Often hopelessness and helplessness are associated with this.
- Bipolar Disorder (2.8%, onset 25 years) – previously known as manic depressive disorder. Patients will often experience extreme mood swings from completely elated to mania to depression but will have long periods of normal moods in between.
- Postpartum Depression(21.9%) -depression during the first postpartum year. The “baby blues” are common after birth however if lasting longer than two weeks, depression is considered.
- Seasonal Depression also known as SAD – major depression with seasonal patterns. Fall and winter months are popular because there is less sunlight.
Causes and risks of depression include the following; a breakup, separation or divorce, poverty, loss of job, accidents with long term disability, bullying, crime victim, long term or chronic illnesses, death, birth, side effects of medications, other mental disorders, intoxication or withdrawal, hormonal changes, lack of sunlight, long term caregivers, family members with depression, people with more emotional personalities, abusive childhoods, females. Medical conditions that are known to cause depression are Parkinson’s disease, Huntington’s disease, traumatic brain injuries, strokes, hypothyroidism, lupus and other autoimmune disorders. Depression is caused by changes in natural brain chemistry. The main neurotransmitter that is involved is serotonin (although dopamine is likely involved too).
To be diagnosed with clinical depression, a person must have one of these two symptoms every day for a minimum of two weeks: an unusually sad mood or loss of enjoyment and interest in activities that used to be enjoyable. Other general symptoms include lack of energy, excessive tiredness, worthlessness, guilt when really not at fault, excessive thoughts about death or wishes to be dead, difficulty concentrating, moving slowly, agitation, sleeping too much or too little, and eating too much or too little.
Symptoms of depression can be further broken down to emotional, thoughts, behavioral, or physical. Emotions that may present are sadness, anger, guilt, lack of emotion, helplessness, hopelessness or irritability. Thoughts include self criticism, self blame, confusion, death and suicide, and impaired memory. Behavior includes crying, withdrawing, neglect of responsibilities, poor appearance and hygiene, illicit drug and alcohol use. Finally, physical symptoms include chronic fatigue, constipation, diarrhea, excessive over or under eating, headaches, loss of sexual desire, unexplained aches and pains.
Treatments include medication, supportive counseling, psychological therapies, and other medical treatments. Medication includes antidepressants with the most popular being selective serotonin reuptake inhibitors. These help the brain make more serotonin available. Supportive counseling is non judgemental listening by a professional (doctors, therapists, counselors, and clergy. Problem solving skills may be taught in this type of counseling. Psychological therapy is Cognitive Behavioral Therapy (CBT). I talked about this in Anxiety. Finally, some medical treatments include the controversial electroconvulsive therapy (ECT). Although ECT has been proven to help in some major depressive cases, the risks out weight the benefits. The major setback with ECT is memory loss.
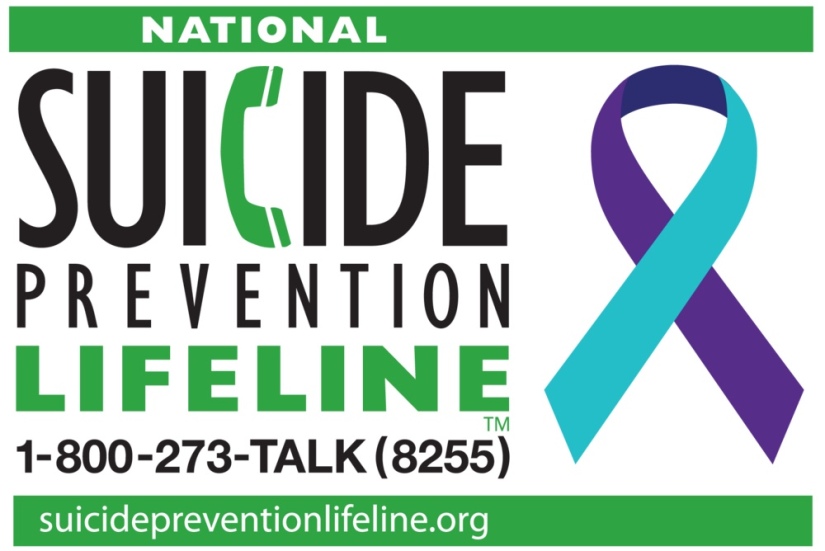
When discussing major depressive disorders, we need to talk about suicide. This may be sensitive for some people so please read at your own comfort. Although suicide will have its own Mental Health Monday, I will briefly highlight it here. Suicide is the 10th leading cause of death in the United States. Males are 4 times more likely to die by suicide but females attempt suicide 3 times more than males. Men typically use more violent ways of suicide such as weapons whereas women use less violent ways such as overdosing. If someone you know is suicidal please ask them the following:
- Are you having suicidal thoughts?
- Are you thinking about killing yourself?
If they answer yes, continue with:
- Do you have a plan on how to kill yourself?
- Have you decided on when you would kill yourself?
- Have you taken any action to secure the objects you need to carry out your plan of suicide?
Please do not leave these people alone. Ask them what they would like to do. Do they want to go to the hospital? Do they already see a provider that they would like to go to? When in doubt call 911.
The best thing we can do is use the words death and suicide and kill. We as a society are very afraid of these words and think if we use these words we will encourage the person to follow through with their plan. This is simply not true. The more comfortable with these words, the more we can help people.
I was diagnosed with depression when I was 23 although honestly I probably was depressed when I was diagnosed with the anxiety when I was 16. My husband moved the Charlotte in January of 2015. I remember that’s when the excessive sadness would occur. No one knew of course because I could get through the day fine but would cry continuously throughout the night. I finally couldn’t handle it anymore and went to see my doctor in June of 2015. I was prescribed Lexapro (SSRI). I remember being so reluctant to take this medication, proving that the stigma had got to me too. But I took it and here we are three and a half years later and i’m still taking it and it’s working great.
Now I must say I am pretty lucky. The first medication they gave me was the one that worked for me. Please do NOT be discouraged if this is not the case for you. All of our brain chemistries are different and sometimes it can take multiple trial and errors for the correct treatment plan to be found for you.
I moved to Charlotte in July of 2015, six months after my husband. Everything was great and I even tried to cut my Lexapro in half. It did not work but the doctor said just give it more time. I was fine until November of that year. I started getting really sad again. Taking care of a sick puppy and working night shift was super hard on my body. My sleep was getting less and less. And of course I did not know anyone in Charlotte. Thankfully, I made a friend named Ben at the dog park. He had a dog named Hercules who played with Maverick every day. I still don’t know to this day if Ben actually listened to me but at least he pretended. Ben and Herc moved to California in January of 2016 which was difficult because I still had not made friends at work that I saw outside of work.
Around March I hit my breaking point. I was so tired and was up for 5 days (later I would learn that this was an episode of mania). I literally was sobbing because I was so tired. I would have done anything to sleep. I went home from working half a shift and ran a bath. I took a Xanax and burned a candle. Still after an hour I was not tired so I took Benadryl. I need to take about 3 times the normal dose of Benadryl to have any effect because of another illness that gave me a tolerance to Benadryl. Well, I finally fell asleep…in the bathtub. I woke up probably about two hours later in freezing cold water by my puppy licking my face. To this day I don’t know how Maverick got into the bathroom because the door was locked (although I was so tired who actually knows). I was coughing as I inhaled water as I slept. Some medical professionals would consider this a passive suicide attempt (will be discussed at a later time). This is when I would realize it was time for professional help. Some people that I talked to asked what could I possibly be depressed about? I had a job, a boyfriend, a dog, parents, a good support system. But the thing is it has nothing to do with this. Although a lack of these things could be attributes to depression they do not actually cause the depression.
A co-worker had seen a therapist and recommended him to me. I went to meet with him and so started my cognitive therapy that would last for about 9 months straight, 11 total. The first three times I went to see him, I cried and it took me 30 minutes just to get out of the door. To me this was finally admitting that I had a problem that I could not manage myself. We worked on so many things. It took no time at all to realize my main trigger which was my lack of ability to control situations. We came up with many plans and back up plans. He gave me a workbook to do which I thought was so silly but when you see your problems on an actual piece of paper it is therapeutic in some weird way. Thankfully, Dr. M helped me and in November I “graduated” therapy. I have had several “tune ups’ with him and will continue to need them as life goes on. I am still on Lexapro to this day. Unfortunately, I will never come off of it as I cannot make serotonin. The best thing my primary doctor told me was “People take antihypertensives and insulin all their life, why does taking antidepressants have to be different?” Having these disorders have helped me become a Mental Health Advocate and if my story helps just one person then it is so worth it.
Thanks for reading! I will post some resources below!
- MentalHealthFirstAid.org
- National Suicide Hotline 1-800-273-8255
- Spanish National Suicide Hotline 1-800-628-9454
- Master of Your Anxiety Workbook https://www.amazon.com/Mastery-Your-Anxiety-Panic-Treatments/dp/0195311353/ref=sr_1_16?ie=UTF8&qid=1535392708&sr=8-16&keywords=anxiety+workbook
- Overcoming Depression https://www.amazon.com/Overcoming-Depression-Cognitive-Approach-Treatments/dp/019537102X/ref=pd_sim_14_4?_encoding=UTF8&pd_rd_i=019537102X&pd_rd_r=d42a1e37-aa22-11e8-8742-1712fd196554&pd_rd_w=1NV3s&pd_rd_wg=lVmWE&pf_rd_i=desktop-dp-sims&pf_rd_m=ATVPDKIKX0DER&pf_rd_p=a180fdfb-b54e-4904-85ba-d852197d6c09&pf_rd_r=NA3PRNH7DRWW8EFRQ2CF&pf_rd_s=desktop-dp-sims&pf_rd_t=40701&psc=1&refRID=NA3PRNH7DRWW8EFRQ2CF